Newsletter Update:
Awhile ago I said that The Healing Newsletter was going to come out every week and that hasn’t happened. The truth is, figuring out what life as a full-time writer/speaker/activist looks like means I need to figure out what I want this newsletter to be. While I’m getting the newsletter’s purpose sorted, it will return to an every other week schedule, on Wednesdays. If you have thoughts on what you would like the newsletter to be, please share them in a comment below.
Why I quit Tamoxifen & Arimidex
Readers of my new book Healing know that I struggled with Tamoxifen, the drug given to women who are pre-menopausal when they are diagnosed with breast cancer. To explain its function as simply as possible, Tamoxifen offers risk reduction by limiting women’s circulating estrogen. Since my tumor had receptors for estrogen (and progesterone), reducing the amount of estrogen in my body would mean less chemical stimulation for any cancer cells. The standard recommendation is that women with estrogen positive breast cancer take Tamoxifen for five years.
That all sounds good, except…starting the drug gave me the worst headache of my life and I spent my first three months on it exhausted and mentally befogged. After that three months the brain fog lifted enough that I could return to nursing work. However, I still was not at my pre-diagnosis level of mental acuity and I had this stealth fatigue that blindsided me a few times every week. I found myself having to constantly weigh my actions against possible future exhaustion. A common concern was, if I take out the trash, will I be too tired to do X later? That is not an exaggeration. Sometimes in the middle of cooking dinner, especially a more elaborate meal, I would need to stop to rest and Arthur would have to take over. My brain would feel so worn out by the evening that I couldn’t do much more than watch television. There’s nothing wrong with that, except that’s not who I was prior to taking Tamoxifen.
Needless to say, that is a hard way to live, and the benefit to me was a relatively small reduction in overall risk. When I put Tamoxifen on the quality of life scale and weighed it against my intermittent fatigue and confusion, the balance was definitely off.

I wanted to do everything possible to keep from ever having cancer again, though, so I kept taking Tamoxifen while constantly complaining that it was ruining my life. Which it kind of was.
Then, a blood test suggested that I was in menopause, and I made the decision to switch from Tamoxifen to the drug Arimidex, which is only effective in post-menopausal women who have had breast cancer, and also reduces risk. I had a pretty detailed conversation with my oncologist about switching and I took Arimidex for a few months and mostly thought it was fine, that maybe I had some extra joint and muscle pain—common side effects—but I could handle it. Then, a new blood test revealed that I was not actually in menopause, that being on Tamoxifen made my lab results look like I was in menopause. Being pre-menopausal meant that Arimidex could not do much to reduce my circulating estrogen.
My summation of what happened next in my cancer treatment is that it went off the rails. My oncologist told me to stop taking Arimidex because it wasn’t helping me. Via a nurse, she also told me to resume Tamoxifen. When I talked to her in person, after saying, “No, I will not restart Tamoxifen,” she said I could stay on Arimidex, but that I would either need a shot to stop my ovaries from producing estrogen, or I could have my ovaries removed, which struck me as a radical solution but that she described as, “It’s just outpatient surgery.”
A few things happened next: 1. I stopped Arimidex and as a result, 2. I had the worst menstrual period of my life (and I’ve had some bad ones) and it lasted a really long time, and hoping for some relief, 3. I agreed to get the shot and got the shot, which caused my blood pressure to really go up (a known side-effect), so that 4. I became incredibly fed up, and 5. decided to switch oncologists.
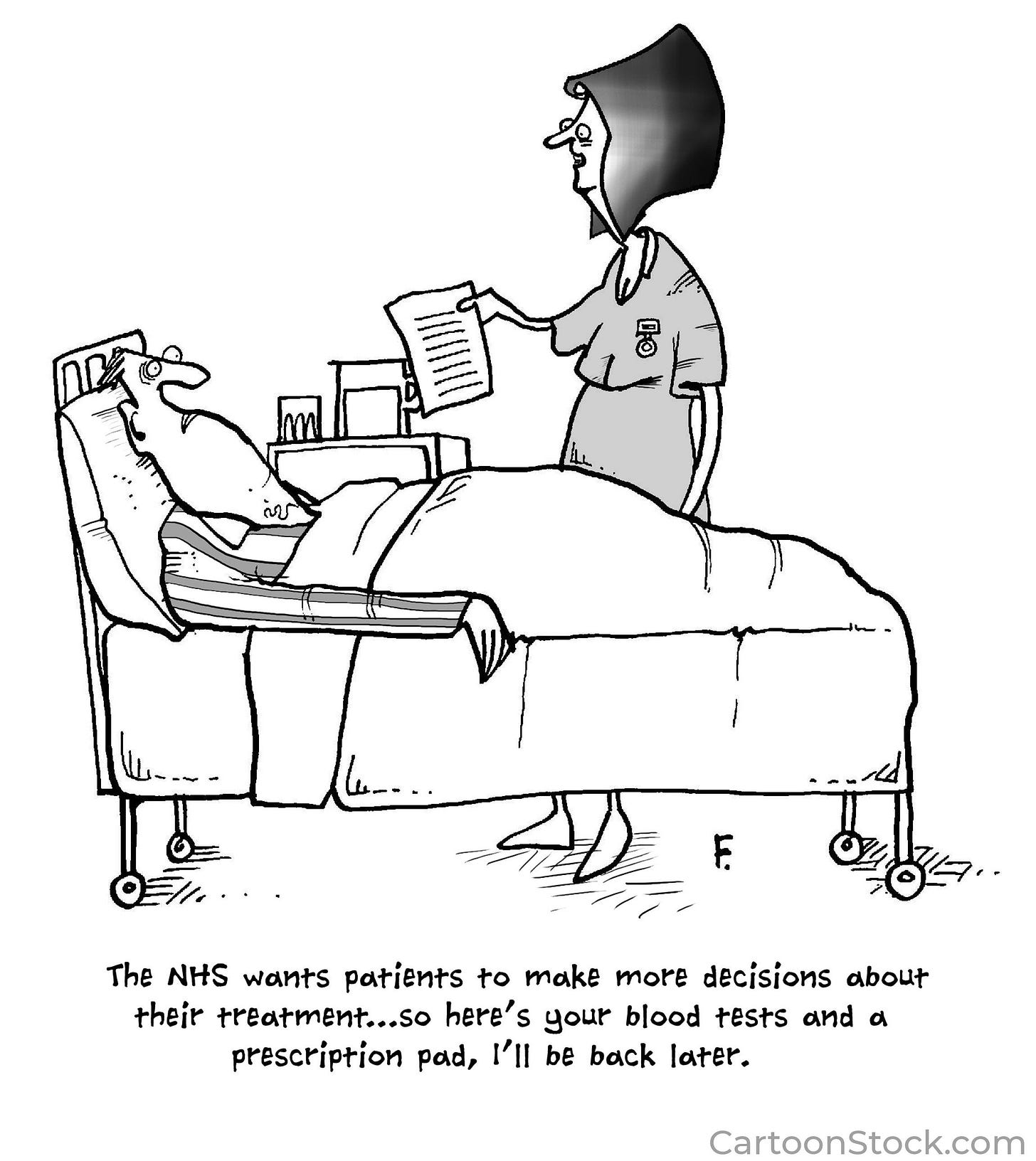
I could say a lot of things about my new oncologist, but here’s what matters: He listens. He listened when I said I wouldn’t take Tamoxifen anymore. He listened when, after he started me on a very low dose of Tamoxifen I said I couldn’t tolerate the side-effects and decided to stop the drug. He suggested we wait and see if I went into full menopause soon-ish and then restart Arimidex. That happened, and then when I couldn’t tolerate the Arimidex (more on that below) and stopped it on my own, he said OK to that. He expressed reservations, an awareness that I wasn’t getting every possible breast cancer risk reduction available to me, but he understood that the choice was ultimately mine. He even used the phrase “shared-decision-making,” which I thought was adorable, even though I could not keep myself from saying, “I’ve heard of that.”
Why, though, did I quit taking Arimidex? A well-known side-effect of Arimidex is bone and joint pain. I’m going to return to when I previously took Arimidex, which included September 2021. During that time, Arthur and I went to Aspen, Colorado for two weeks. He attended workshops at the Aspen Center for Physics and I did what writers do. I also went for a four hour horseback ride and he and I did a pretty arduous hike. At the end of both those experiences I had so much pain I felt physically ill. It felt like someone had picked me up, shaken me really hard, and then put me back down again, leaving my joints loose and out of synch. At the time I thought it was ordinary muscle pain from overtaxing myself: taking too long a ride and too hard a hike when I wasn’t used to either.
Fast forward to a couple months ago when I re-started Arimidex. Pretty quickly I had that same joint and muscle pain, but I had it almost all the time. It is anecdotally acknowledged that post-menopausal women have increased joint pain. A cursory google check suggested that this reality is not well understood, though the chart below from MenopauseNow.com offers one theory:
I put two and two together—my pain from last September and the pain I was having on Arimidex were the same pain, and it hurt quite a bit. Soon, I quit Arimidex. I told my family and I told a few friends. I waited for a scheduled appointment with my new oncologist, which took place last week, and then I told him.
It all ended well, as I already described, in that the doctor listened and validated my choice. It’s almost five years to the day from my initial diagnosis—the mammogram and ultrasound described by the radiologist with just four devastating words: “I see a mass.” My oncologist said that five years is when hormonal therapies usually stop. It seemed like he was trying to convince himself as much as me, but what he said helped. These anti-estrogen drugs do reduce risk, but to me they offered a devil’s bargain: lose yourself to reduce your risk (Tamoxifen); live in pain and reduce your risk (Arimidex). I said no to both drugs out of necessity, but my decision does not make me happy. I’ve increased my risk of having a cancer recurrence because risk reduction took too much away from all the rest of my life.
A bit of recognition:
The Gold Foundation, which “champions humanism in healthcare,” announced their “2022 Gold Foundation Reading List for Compassionate Clinicians” and they included Healing. I’m ecstatic to be on this list and included in such great company. To learn more, and see the entire list, read here.
Alas, Arthur caught Covid last week, possibly at a Pirate’s Game. He is doing OK enough and so far I am Covid-free. The point is, stay safe—this wily virus is still causing trouble.
Hugs to all,
Theresa








Theresa: What I would like to see in your Newsletter
1. Continued personal stories about you. Your readers have come to know you intimately and to care for you, as well.
3. Continued discussion about the challenges we all face in health care. For example, the difficult in navigating our own care. Or how so many choices regarding Covid (for example, immunization in very young children) are not black and white.
Theresa, I so strongly endorse your choice to stop taking medications that were making you miserable and brought you only a negligible benefit. Too often, medical professionals think that because we can do something, we ought to, no matter the consequences. But really the correct approach is to balance risks and benefits and decide when an intervention is worth it to us.
Here’s a personal story: Between ages 13 and about 30, I used to faint, sometimes several times per day. As I’m sure you know, this is a very common problem in tall skinny teenaged girls, especially if they have slow heartbeats (mine was under 60bpm) and low blood pressure (mine was 90/40!). After two cardiac catheter studies, my cardiologist put me on Norpace, which had to be begun in the hospital because it has the rare side effect of cardiac arrest, which will appear in the first 48 hours or not at all. The whole process of getting on this drug was painful, expensive, and disruptive. Then I started taking the drug, and it gave me such a dry mouth that I could no longer sing. I decided that I would rather be able to sing even if it meant fainting a few times a day, and I refused to take the medication (it was also expensive, and I thought it was morally wrong to impose that cost on my mom’s teachers’ HMO). My doctor objected but conceded that it was my choice. Yes! It is always our choice, and we often know better than our doctors what makes sense for us!
I hope Arthur’s experience with Covid will be like mine--cold symptoms and no sense of smell for a couple of days and then totally fine--and that you don’t get it! But thanks to the vaccines and boosters, most people I know (even my parents) have an easy time of it. Hooray for the vaccines!